Pharmacy is the act or practice of preparing, preserving, compounding and dispensing drugs. According to the National Association of Pharmacy Regulatory Authorities (NAPRA), as of 1 January 2024, there were approximately 11,712 community pharmacies and 46,860 pharmacists in active practice across Canada.
Background
Louis Hébert, one of the first settlers of New France, was a pharmacist from Paris. From the time he settled in Quebec (1617) until 1750, when the first medical legislation by Intendant François Bigot was promulgated, there was little regulation of the health professions in New France. For the next 120 years, efforts to obtain more specific and effective legislation for the control of drug distribution were integrated into medical regulations and were largely ineffectual. A number of pharmacists' organizations were formed in both Upper Canada and Lower Canada during this time in an attempt to establish pharmacy legally as a profession. These groups were short lived; there was no permanent national organization of Canadian pharmacy until the Canadian Pharmaceutical Association was founded in 1907 (renamed the Canadian Pharmacists Association in 1997).
Until Confederation, 1867, efforts by pharmacy organizations to obtain appropriate regulation by federal legislation were unsuccessful. With the creation of the provinces of Quebec and Ontario, pharmacy Acts were passed (in 1870 and 1871, respectively) granting self-government to the profession. These Acts served as models for the rest of Canada; each province has now passed similar legislation to regulate the practice of the profession within its borders. Under this legislation, the professional association issues the licences to practise and supervises its members.
Nevertheless, significant differences exist from province to province. Registration in any one province qualifies a pharmacist to practise also in the Yukon and the Northwest Territories, but not in other provinces, because the requirements of each province must be met separately. In response to this situation, the Pharmacy Examining Board of Canada was formed in 1963 under federal statute to establish academic qualifications acceptable to participating provincial licensing bodies.
Education and Training
Pharmacists no longer learn their profession through an apprenticeship system. All provinces require pharmacists to obtain a baccalaureate degree in pharmacy for licensure. Faculties of pharmacy are located at Dalhousie University, the Université de Montréal, the Université Laval, University of Toronto, University of Waterloo, University of Ottawa, University of Manitoba, Memorial University of Newfoundland, University of Saskatchewan, University of Alberta and University of British Columbia.
Courses in basic biological and physical sciences are a required prerequisite to professional pharmacy courses and the program of studies that includes supervised practical experience. Research has become important in the pharmacy colleges because advances in drug therapy arise primarily from work carried out in industry and the universities. (See also Medical Research.) All Canadian faculties of pharmacy provide graduate work at the master's and doctoral level for students seeking careers in teaching, research, industry, hospital pharmacy and other specialized areas.
Roles and Activities
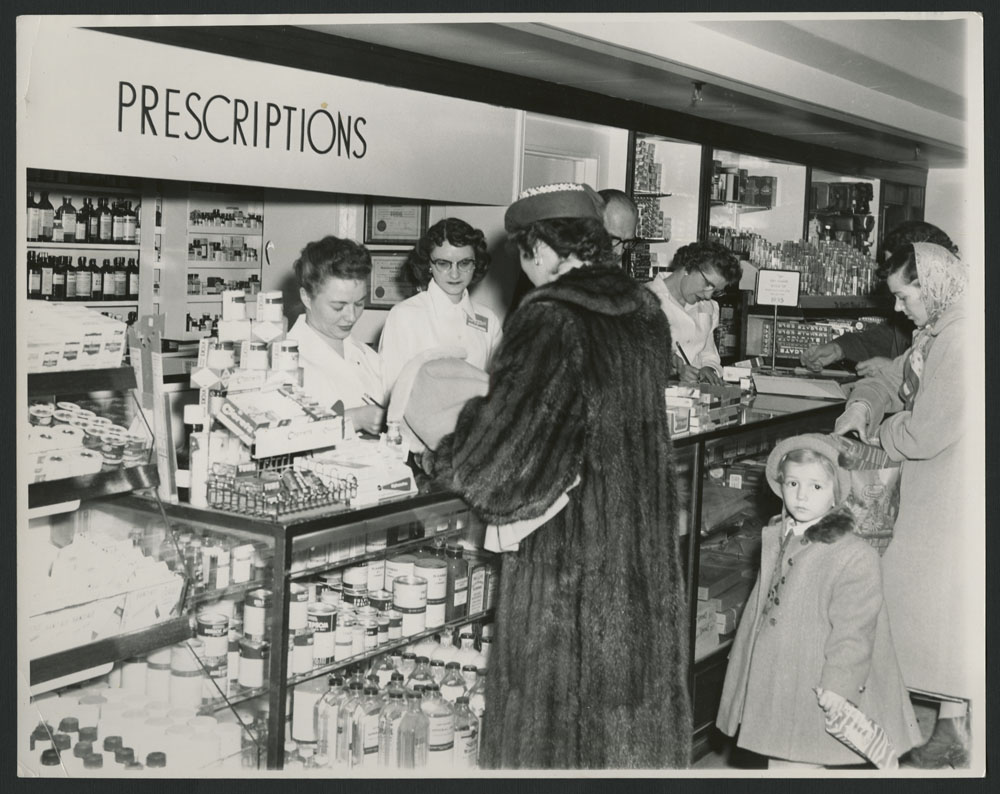
About a third of Canadian pharmacies are large establishments (frequently part of chain stores and franchise operations), selling a variety of merchandise in addition to providing prescriptions and health needs.

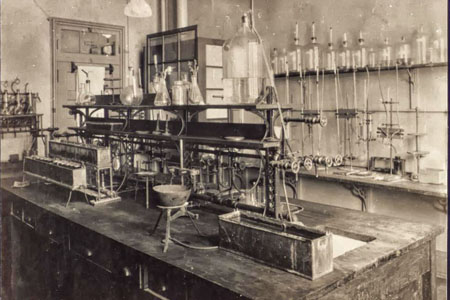
The professional practice of pharmacy has changed dramatically over the years. Pharmacists now dispense a vast array of complex, potent and specific medicinal agents (the federal government has enacted regulations dealing with the quality, safety and efficacy of therapeutic agents, and specifying the terms under which certain potent and addictive drugs must be handled). The preparation of these pharmaceuticals requires special techniques of formulation and analysis that are available more efficiently and economically in the elaborately equipped laboratories of industry; therefore, most of the pharmaceuticals dispensed today are obtained by the pharmacist in the finished form.
The pharmacist's role has changed from that of compounder to that of a supervisor of drug regimens and a consultant to the other health professions and to the public on drug usage. This transition was initially developed in hospitals, where it is now well established. More recently, this concept of clinical pharmacy has been extended to ambulatory patients. The community pharmacist has frequent contact with patients receiving medication and is thus able to protect against drug interactions, toxicities, side effects, allergic reactions and other untoward responses. Most pharmacies today maintain a patient-record system, usually computerized, to help the pharmacist follow the progress of drug treatment. (See also Computer Communications.)

 Share on Facebook
Share on Facebook Share on X
Share on X Share by Email
Share by Email Share on Google Classroom
Share on Google Classroom